
In case you missed it, our pelvic health specialists at CORA recently reviewed the anatomy of your pelvic floor (men + women) to provide you with a deeper knowledge and understanding of the different situations where leakage can occur. Our goal? To make sure you are feeling equipped with basic information that will help you control stop gaps with facts about your pelvic health.
Now that you know the basics, we encourage you to keep reading for simple ways you can treat incontinence with conservative interventions!
Behavioral and lifestyle adjustments in conjunction with pelvic floor muscle training (PFMT) can result in positive outcomes.
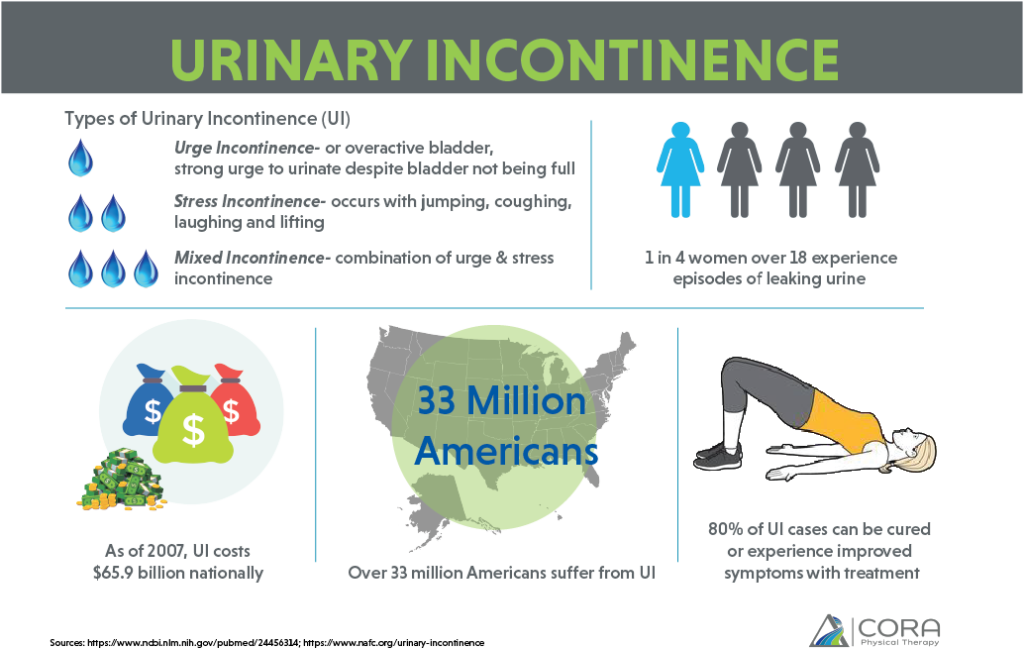
As defined by the International Continence Society (ICS), urinary incontinence is the involuntary loss of urine. Simple, right? Well, not exactly. What that definition does not tell us is that this disorder can be temporary, as in, the first couple weeks after childbirth or surgery, or it can be a chronic problem lasting months to years and even, for some, a lifetime.
You may be familiar with a few of the many coded statements used to describe the experience of incontinence:
“Let me use the bathroom just in case, [for an hour long trip].”
“It’s only a sprinkle when I lift.”
“I have to be careful how hard I laugh.”
The chances are if you have ever said these words or even thought them, you are suffering from Urinary Incontinence (UI).
What’s the Big Deal?
You might be thinking, “this will never happen to me,” “I just wear a liner,” “it’s no big deal,” or “no one really needs to know.” But it is a big deal, and there are interventions for your incontinence supported by surgical procedures or non-surgical, more conservative treatments such as physical therapy.
A Cochrane review published in 2016 determined that 1/4 of all adult women have urinary incontinence, and its prevalence increases with age. The good news is that most cases of UI can be cured or experience improved symptoms with proper diagnosis and treatment protocols.
“The greatest obstacle toward obtaining treatment appears to revolve around reluctance to disclose the condition.”
As is often the case when dealing with health and wellness issues, there are direct and indirect impacts as a byproduct of UI. Indirect impacts may include psychological factors like depression, isolation, decreased self-esteem and work related difficulties that can put a serious dent in your quality of life. Many living with UI find themselves limiting their socialization for fear of embarrassment, while others map out errands to coordinate frequent bathroom stops.
We’ve all seen Brooke Burke’s commercial for Poise pads, and we’re all too familiar with products on the market for incontinence with brands like Tena, Always and Depends engrained in the fabric of pop culture. However, it’s important to know that treatment options do exist…and the sooner it’s addressed, the better!
Finding the most effective course of action begins with identifying which one of the three types of incontinence you’re experiencing: stress, urge or mixed incontinence. Armed with this information, your healthcare provider can recommend the appropriate intervention—conservative methods or surgical treatment options.
Treating Incontinence with Conservative Interventions
Although sometimes surgery may be necessary, there are a number of conservative, non-surgical interventions—including physical therapy—that can lessen symptoms and improve quality of life. A review in the Cochrane Library by Alex Pollock et al lists some conservative treatment protocols that have proven effective, depending on the type of UI.
- Education / Behavioral / Lifestyle Advice: Monitor diet and fluid intake, and implement voiding intervention including timed voiding and teaching healthy bowel management.
- Physical Therapy: Pelvic floor muscle training, exercises and manual therapies that include biofeedback and stimulation.
- Psychological Therapy: Cognitive behavioral therapies and mindfulness based therapies.
- Mechanical Devices: Pessaries and self-catheterization, to name a couple.
- Complementary therapies: Acupuncture, reflexology, hypnotherapy and the Bowen Technique
- Others: Yoga, core stability training and breathing exercises; hypopressive exercise, which is a newer technique with less research backing its effectiveness.
And lastly, you can always talk to your doctor or physical therapist about the use of medication as part of your treatment plan.
Muscle Control and Coordination Makes All The Difference
Not every part of our voiding reflexes and elimination practices can be voluntarily controlled by us, but the parts that can be controlled become stop gaps against unwanted leakage or incontinence. As musculoskeletal specialists, physical therapists are skilled in the rehabilitation of muscle control and coordination. In the case of the pelvic floor muscles, PTs with special training in pelvic health can help bring awareness to these muscles and their proper function. We teach patients how to strengthen the muscles and coordinate their contractions or teach relaxation techniques for the appropriate functions. We can even address some of the behaviors that may exacerbate your symptoms.
Your therapist or healthcare provider is well-trained to help you safely review medications that may be exacerbating the symptoms, or identify foods that may be triggering episodes of incontinence because they are irritating your bladder. As PTs, we also know how to identify behaviors that sabotage your success as well as the musculoskeletal factors that may be decreasing your ability to control your bowel movements. We use this knowledge to apply behavioral modification techniques that can minimize occurrence, including food and drink intake and timed voiding. This approach addresses muscles and teaches techniques for strengthening, relaxation and coordination for successful voiding.
How CORA Physical Therapy Can Help
Significant studies over the years have supported the use of physical therapy services, namely pelvic floor muscle therapy for cure or improvement of incontinence. There are also positive outcomes with behavioral and lifestyle adjustments in conjunction with pelvic floor muscle training (PFMT) that can improve your quality of life.
Evidence suggests that this assessment and nonsurgical management of UI is applicable to the standard patient; however, therapy should always be tailored to individual patients’ needs and circumstances. So if you find yourself saying any of those statements mentioned above, it may be time for you to reach out to us here at CORA Physical Therapy for a quick consultation so we can get you back to living your life free of stressful or embarrassing urges.
